
The Latest and greatest treatments for IBD: What to believe
What’s the best IBD medicine for me? Confusion on television and in your inbox....
See moresign up for our newsletter
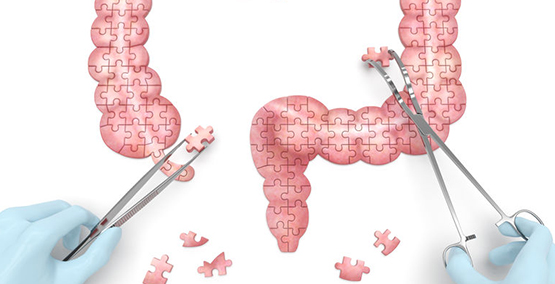
SubscribeThe short answer is that we don't know yet. But we actually know a great amount. Everyone has an immune system that responds to and fights off infection. Some people don't fight off infections as well as others. And some people seem to over-respond, in ways that their immune system ends up attacking their own bodies. That over-response is considered an auto-immune response. And that whole process often ends up in the inflammation that's part of Crohn's disease and ulcerative colitis (UC).
To take that a step further, how we respond has to do with our genes. Usually several of our genes, the ones that regulate the barrier between our intestines and what's coming through it (the food and all the chemicals and bacteria that come into our mouths every day. They also get help from the normal population of organisms that live in our intestinal tracts (it used to be called the intestinal flora, now it's usually called the "microbiome"). A healthy microbiome helps to protect against infections and other injuries as well.
A Mouse Model Can Help Us Understand IBD
Dr. Balfour Sartor was able to show this in mice. He took genetically bred mice with the absence of an immune factor and exposed them to bacteria. The mice developed an illness similar to IBD in humans. If he took the same mouse but never gave them the bacteria, they remained healthy. And if he gave the bacteria to healthy mice, nothing happened.
In humans, we know the same thing happens, but perhaps with a variety of immune defects caused by the person's gene type, allowing something to trigger the inflammation. For most older children, teens and adults, the genes are thought to only count for 8-20% of why a person gets IBD. Because there is a genetic part, IBD can run in families, though most people who have IBD do not have an immediate family member with IBD.
At present, the primary triggering event has not been defined. It may not be that there is a single cause for all people. Most likely, there's a variety of infections and other triggers, since we think that some medications (like ibuprofen and other anti-inflammatory medicines) can also act as triggers by destroying part of the protective layers in the intestine.
As a result, there's a lot of research on the immune factors and the triggers, with many of the studies are focusing on the microbiome and the protective layers of the intestine, since they may play an important role in protecting certain individuals and allowing others to get IBD. We know too that the intestinal population is certainly affected by diet, so nutrition is beginning to get more research and clinical attention as well, especially since IBD is on the increase around the world.
This article, as well as all others, was reviewed and edited by a member of our Medical Advisory Board.
Subscribe Be the first to know